Pain Management for Rheumatoid Arthritis: Top Strategies Revealed

Introduction
Living with rheumatoid arthritis can turn simple daily tasks into difficult challenges. This long-lasting autoimmune condition affects millions of people around the world, causing constant joint pain, stiffness, and swelling that can greatly affect one's quality of life.
Pain management is a key part of treating rheumatoid arthritis. Whether you're feeling symptoms in your knees, feet, or other joints, it's important to find effective ways to relieve the pain so you can stay independent and healthy.
This detailed guide will show you proven methods for managing rheumatoid arthritis pain, such as:
- Targeted medication options
- Physical therapy techniques
- Alternative therapies
- Home remedies
- Lifestyle changes
Whether you have severe rheumatoid arthritis or mild symptoms, you'll find specific solutions that can help lessen discomfort and improve joint movement. We'll look at both traditional medical treatments and natural alternatives, giving you a complete set of tools for managing pain.
Let's explore the most effective strategies that can help you take back control of your daily activities and improve your quality of life.
Understanding Rheumatoid Arthritis and Its Pain Mechanisms
Rheumatoid arthritis (RA) is a complex autoimmune condition where your immune system mistakenly attacks healthy joint tissue. This chronic disease causes persistent inflammation in your joints, leading to progressive damage and deterioration.
Key Characteristics of RA:
- Symmetrical joint involvement (affects both sides of the body)
- Morning stiffness lasting longer than one hour
- Persistent inflammation in multiple joints
- Progressive joint damage without proper treatment
Your daily experience with RA typically includes several distinct symptoms:
- Tender, warm, and swollen joints
- Reduced range of motion
- Fatigue and general weakness
- Low-grade fever during flare-ups
- Joint deformity in advanced stages
The pain you experience in RA comes from multiple sources. Systemic inflammation is the main cause, triggering a series of inflammatory substances that make nerve endings in your joints more sensitive. This process creates a heightened pain response, making your joints increasingly sensitive to movement and pressure.
Pain Mechanisms in RA:
- Inflammatory Pain: Caused by active inflammation in joint tissues
- Nociceptive Pain: Results from actual tissue damage
- Neuropathic Pain: Develops from nerve damage or dysfunction
- Central Sensitisation: Your nervous system becomes more responsive to pain signals
The inflammatory process in RA creates a cycle that keeps going. As inflammation damages joint tissues, it releases more inflammatory substances, leading to more pain and tissue destruction. This cycle explains why early intervention with appropriate medication is crucial in managing RA symptoms and preventing joint deterioration.
Your pain experience can vary throughout the day and may become worse during periods of increased disease activity, known as flares. These fluctuations in pain levels reflect the changing nature of RA's inflammatory processes and highlight the need for comprehensive pain management strategies.
Comprehensive Pain Management Strategies for Rheumatoid Arthritis
Managing rheumatoid arthritis pain requires a multi-faceted approach tailored to each patient's specific needs. A successful pain management strategy combines both pharmacological and non-pharmacological treatments to achieve optimal results.
1. Pharmacological Approaches to RA Pain Management
Modern medicine offers several effective medications to combat RA pain and inflammation. These treatments work through different mechanisms to provide relief and slow disease progression:
- First-line Medications: Your doctor might prescribe NSAIDs or DMARDs as initial treatment options
- Advanced Therapies: Biological agents target specific components of the immune system
- Combination Therapy: Multiple medications can work synergistically for enhanced pain relief
The choice of medication depends on several factors:
- Disease severity
- Individual response to treatment
- Presence of other medical conditions
- Risk factors for medication side effects
Your healthcare provider will create a personalised treatment plan based on these factors. Regular monitoring helps ensure the effectiveness of your medication regimen while minimising potential side effects.
The pharmaceutical approach to RA pain management has evolved significantly with new research and drug development. Treatment options now extend beyond traditional pain relievers to include targeted therapies that address the root causes of inflammation and joint damage.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs) in RA Treatment
NSAIDs are a key part of managing pain caused by rheumatoid arthritis (RA). They work in two ways: reducing inflammation and relieving pain. Here are some common NSAIDs that doctors often prescribe:
- Ibuprofen (Brufen, Nurofen)
- Naproxen (Naprosyn)
- Diclofenac (Voltarol)
- Celecoxib (Celebrex)
These medications work by blocking certain enzymes that produce prostaglandins, which are substances that cause inflammation, pain, and fever. The pain-relieving effects usually start within a few hours, making NSAIDs useful for quick relief.
Benefits of NSAIDs:
- Fast-acting pain relief
- Reduced swelling in joints
- Less stiffness in the morning
- Improved physical abilities
- Available in different forms such as tablets, gels, and patches
Potential Side Effects:
- Stomach ulcers and bleeding
- Increased blood pressure
- Changes in kidney function
- Higher risk of heart issues
- Interactions with other medications
Your doctor may suggest taking NSAIDs with food or prescribe medication to protect your stomach from side effects. It's important to regularly monitor your kidney function and blood pressure to ensure it's safe for you to use NSAIDs long-term. Some patients find relief from using topical NSAID preparations, which can provide targeted relief with fewer side effects throughout the body.
Disease-Modifying Antirheumatic Drugs (DMARDs) and Their Role in Managing RA Pain
Disease-Modifying Antirheumatic Drugs (DMARDs) represent a crucial advancement in rheumatoid arthritis treatment. These medications work by targeting the root cause of RA: the immune system's attack on healthy joint tissue.
Traditional DMARDs include:
- Methotrexate - The gold standard first-line treatment
- Sulfasalazine
- Hydroxychloroquine
- Leflunomide
DMARDs function by suppressing the immune response responsible for joint inflammation and damage. This suppression leads to:
- Reduced joint swelling
- Decreased pain levels
- Slowed disease progression
- Prevention of joint deformities
The pain-relieving effects of DMARDs typically develop over several weeks to months. Your rheumatologist might prescribe these medications alone or in combination for enhanced effectiveness.
While DMARDs don't provide immediate pain relief like NSAIDs, their long-term benefits make them indispensable in RA treatment. Research shows that early DMARD therapy can:
- Prevent irreversible joint damage
- Reduce the need for joint surgery
- Improve quality of life
- Maintain joint function
Side effects vary among different DMARDs. Regular blood tests help monitor your response to treatment and detect potential complications. Your doctor will adjust the dosage based on your specific needs and treatment response.
DMARDs require careful monitoring and patience as their full benefits develop. Many patients notice significant improvements in pain levels and joint function within 3-6 months of starting treatment.
Biologics, Targeted Therapies, and Emerging Options for RA Pain Relief
Biologic therapies represent a significant advancement in rheumatoid arthritis treatment. These specialised medications target specific components of the immune system responsible for inflammation and pain.
Common biologics include:
- TNF inhibitors (adalimumab, etanercept)
- B-cell inhibitors (rituximab)
- T-cell inhibitors (abatacept)
- Interleukin inhibitors (tocilizumab)
These medications work by blocking specific proteins that trigger inflammation in your joints. Research shows biologics can reduce pain levels by up to 50% in many patients within the first few months of treatment.
Janus kinase (JAK) inhibitors are a newer class of targeted synthetic DMARDs that work inside your cells to disrupt inflammatory signalling. Popular JAK inhibitors like tofacitinib and baricitinib offer additional benefits:
- Oral administration (unlike injectable biologics)
- Rapid onset of action
- Effective pain relief
- Improved physical function
Your doctor might prescribe biologics or JAK inhibitors if traditional DMARDs haven't provided adequate relief. These medications can be used alone or combined with other treatments for enhanced effectiveness.
Recent clinical trials are exploring new therapeutic targets and delivery methods. Promising developments include:
- IL-6 inhibitors
- GM-CSF receptor antagonists
- Novel small molecule inhibitors
2. Non-Pharmacological Approaches to Managing RA Pain Effectively
A comprehensive RA pain management strategy extends beyond medication. Non-pharmacological approaches play a vital role in reducing discomfort and improving daily function for RA patients. These methods work synergistically with prescribed medications to create a robust pain management system.
Research shows that combining medication with non-drug therapies can lead to:
- Reduced joint stiffness
- Improved range of motion
- Better sleep quality
- Enhanced daily function
- Decreased reliance on pain medication
Non-pharmacological approaches include physical therapy, exercise programmes, hot and cold therapy, assistive devices, and lifestyle modifications. These methods empower patients to take active control of their pain management journey while supporting their prescribed medical treatments.
The effectiveness of these approaches varies among individuals, making personalised treatment plans essential. Working with healthcare providers to develop a tailored non-pharmacological strategy ensures optimal pain management results.
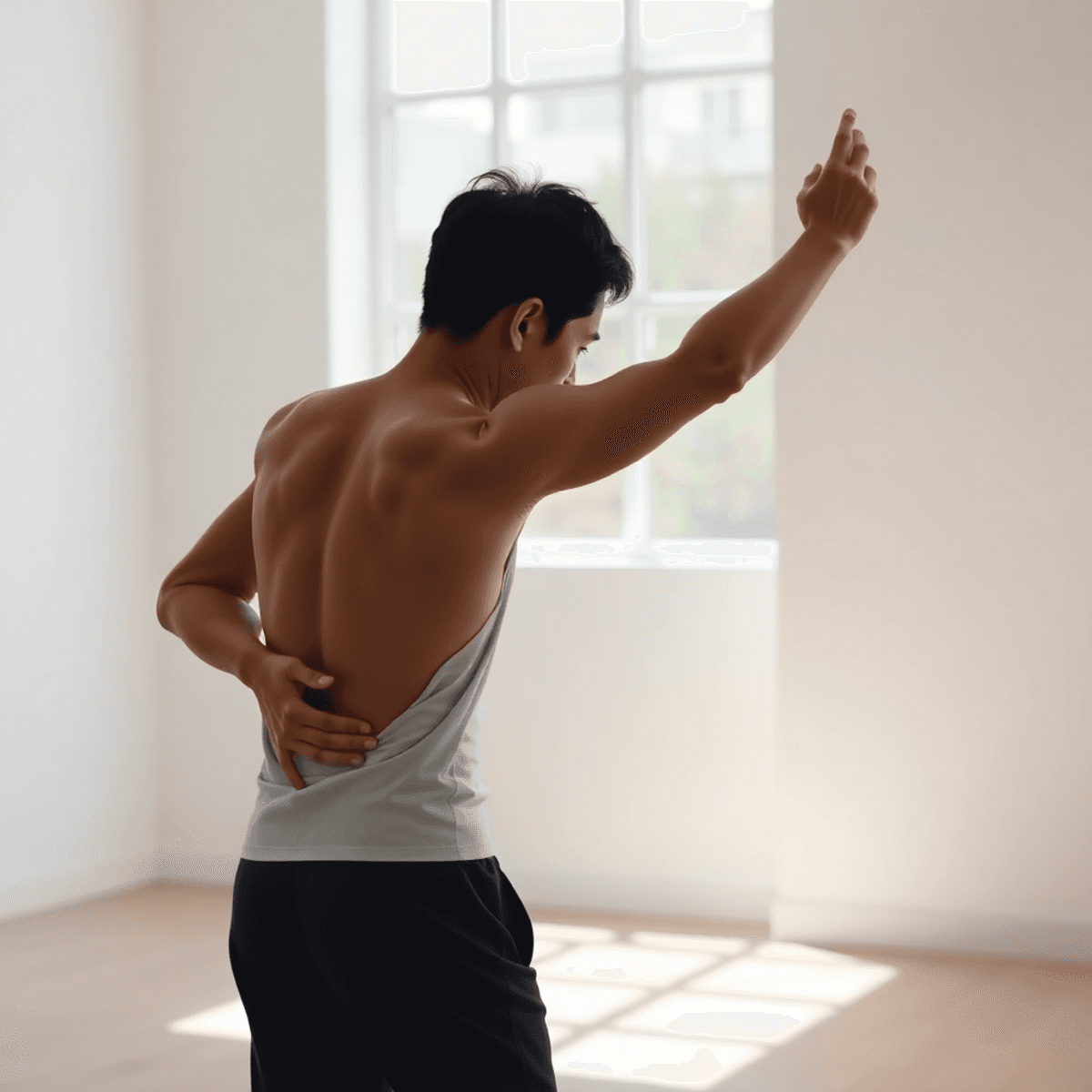
The Benefits of Physical Therapy and Exercise in Alleviating RA Discomfort
Physical therapy and tailored exercise programmes are effective methods for managing rheumatoid arthritis pain. Following a structured exercise routine can greatly enhance joint movement and lessen stiffness while also strengthening muscles to provide support to affected joints.
Key exercises proven to help RA patients include:
- Range-of-motion exercises - gentle stretching movements that help maintain joint flexibility
- Strengthening exercises - resistance training to build muscle support around joints
- Low-impact aerobic activities - swimming, cycling, or walking to improve cardiovascular health
- Balance exercises - activities that enhance stability and reduce fall risk
Research indicates that consistent physical activity can reduce pain intensity by as much as 30% in RA patients. An experienced physiotherapist can develop a customised exercise programme that takes into account your specific joint limitations and pain levels.
Benefits of regular exercise for RA patients:
- Reduced joint stiffness and improved flexibility
- Increased muscle strength and joint stability
- Better sleep quality and reduced fatigue
- Improved cardiovascular health
- Lower inflammation levels
- Enhanced mood and reduced stress
It's important to start slowly and gradually increase the intensity of your exercises to avoid injury and ensure long-term progress. Many patients find water-based exercises particularly helpful as they allow for movement with minimal stress on the joints.
Exploring Alternative Therapies: Heat, Cold, Splints, and Aids for RA Pain Relief
Temperature therapies serve as effective tools in managing rheumatoid arthritis discomfort. Heat therapy relaxes muscles and increases blood flow to affected joints, reducing morning stiffness and pain. You can apply heat through:
- Warm baths or showers
- Heating pads
- Paraffin wax treatments
- Warm compresses
Cold therapy helps decrease inflammation and numb pain signals. Apply cold treatments through:
- Ice packs
- Cold compresses
- Cooling sprays
- Cold water immersion
Proper timing of these treatments matters - heat works best for morning stiffness, while cold therapy helps during acute flare-ups.
Splints and mobility aids play a crucial role in joint protection and pain management:
- Wrist splints stabilise joints during activities
- Finger splints prevent deformities
- Walking sticks reduce pressure on weight-bearing joints
- Grab rails assist with daily activities
- Modified utensils make tasks easier on hands
These aids help maintain independence while protecting your joints from additional stress. Your occupational therapist can recommend specific devices based on your needs and lifestyle.
Remember to alternate between heat and cold therapies based on your symptoms, and always wrap temperature treatments in a towel to protect your skin.
Over-the-Counter Treatment Options: Best OTC Medicines for Rheumatoid Arthritis Pain Relief
Several effective over-the-counter medications can help manage rheumatoid arthritis pain. Here's what you need to know about the most reliable OTC options:
1. NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
- Ibuprofen (Advil, Motrin) - Reduces inflammation and pain, available in various strengths
- Naproxen sodium (Aleve) - Provides longer-lasting relief, requiring fewer doses throughout the day
- Aspirin - Traditional pain reliever with anti-inflammatory properties
2. Topical Pain Relievers
- Capsaicin creams - Derived from chilli peppers, these creams create a warming sensation that interrupts pain signals
- Menthol-based rubs - Provide cooling relief and temporary pain reduction
- Diclofenac gel - Available OTC in some countries, combines anti-inflammatory properties with local application
3. Acetaminophen (Paracetamol)
- Helps manage pain without reducing inflammation
- Suitable for combining with other treatments
- Lower risk of stomach irritation compared to NSAIDs
Safety note: While these medications are available without prescription, they carry potential risks. Long-term use of NSAIDs can lead to stomach problems or increased cardiovascular risks. Always follow dosage instructions and consult your healthcare provider about the most suitable OTC options for your specific situation.
4. Complementary OTC Supplements
These supplements may provide additional support for managing RA symptoms:
- Glucosamine and chondroitin supplements
- Fish oil capsules
- Vitamin D supplements
These OTC options work best as part of a comprehensive treatment plan under medical supervision. Regular monitoring helps ensure their safe and effective use while managing RA symptoms.
Home Remedies for Rheumatoid Arthritis Pain Relief: Natural Treatments That May Help Manage Symptoms at Home
Natural remedies can complement your prescribed RA treatment plan, offering additional relief from pain and inflammation. Here are science-backed home remedies you can try:
Dietary Supplements
- Turmeric: Contains curcumin, a compound with potent anti-inflammatory properties
- Omega-3 fatty acids: Found in fish oil, these help reduce joint stiffness and tenderness
- Ginger: Reduces inflammation and provides natural pain relief
- Green tea: Rich in antioxidants that may help reduce joint damage
Lifestyle Modifications
- Regular gentle stretching exercises
- Stress management through meditation or deep breathing
- Adequate sleep (7-9 hours) to support immune function
- Maintaining a healthy weight to reduce joint stress
Natural Topical Applications
- Essential oils (eucalyptus, lavender) mixed with carrier oils
- Warm compress with Epsom salts
- Apple cider vinegar soaks for affected joints
Dietary Changes
- Anti-inflammatory foods (berries, leafy greens)
- Limited processed foods and refined sugars
- Increased consumption of whole grains and lean proteins
Important: Always consult your healthcare provider before starting any new natural remedy. These treatments should complement, not replace, your prescribed medication regime. Some natural supplements can interact with RA medications or affect their effectiveness.
FAQs
What is rheumatoid arthritis and how does it cause pain?
Rheumatoid arthritis (RA) is a complex autoimmune condition characterized by symmetrical joint involvement, where inflammation in the joint tissues leads to inflammatory pain. This pain is primarily caused by active inflammation that affects both sides of the body.
What are the pharmacological approaches to managing pain in rheumatoid arthritis?
Pharmacological approaches include the use of Nonsteroidal Anti-inflammatory Drugs (NSAIDs), which help reduce inflammation and pain, Disease-Modifying Antirheumatic Drugs (DMARDs) that alter the disease progression, and biologics that provide targeted therapy for RA pain relief.
How can physical therapy and exercise help with rheumatoid arthritis pain?
Physical therapy and tailored exercise programs are effective in alleviating discomfort associated with RA. They help improve joint function, increase mobility, and strengthen muscles around affected joints, ultimately reducing pain.
What over-the-counter treatment options are available for rheumatoid arthritis pain relief?
Several effective over-the-counter medications can help manage RA pain, including NSAIDs like ibuprofen, topical pain relievers such as capsaicin creams, acetaminophen for general pain relief, and complementary OTC supplements that may provide additional support.
What lifestyle modifications can assist in managing rheumatoid arthritis symptoms?
Lifestyle modifications include regular gentle stretching exercises, stress management techniques, dietary changes that focus on anti-inflammatory foods like berries and leafy greens, and using natural topical applications such as essential oils mixed with carrier oils.
Are there natural remedies that can help relieve rheumatoid arthritis pain at home?
Yes, natural remedies can complement prescribed RA treatments. Options include dietary supplements like turmeric for its anti-inflammatory properties, as well as home remedies such as heat or cold therapies to alleviate discomfort.