Non-Opioid Pain Control Strategies: Tips for Managing Chronic Pain

Introduction
Chronic pain affects millions globally, posing a significant challenge in healthcare. Conditions like osteoarthritis, diabetic neuropathy, and fibromyalgia contribute to this pervasive issue. Effective pain management strategies are crucial for enhancing quality of life. Traditionally, opioids have been considered strong pain meds; however, their use carries substantial risks.
- Opioid Limitations and Risks:
- Addiction and Dependency: Opioids are highly addictive, leading to a risk of dependency.
- Side Effects: These include sedation, nausea, and increased tolerance over time.
The search for the best painkillers without opioids has become essential. Non-opioid strategies offer promising alternatives for atopic pain relief. Exploring these methods provides hope for safer, effective pain management solutions.
One such alternative involves the use of all-natural ingredients, which have shown potential in providing relief from chronic pain. These natural remedies not only help in managing pain but also come with fewer side effects compared to traditional medications. As we delve into various non-opioid options, the focus remains on finding viable treatments that minimize risks while effectively managing chronic pain.
Understanding Chronic Pain Conditions
Chronic pain, typically defined as pain persisting for more than 12 weeks, affects millions worldwide and represents a significant challenge in healthcare. This persistent pain can result from various underlying conditions, leading to diverse experiences and management needs among sufferers.
Common Types of Chronic Pain
1. Osteoarthritis
This degenerative joint disease is characterized by the breakdown of cartilage, causing joint stiffness and pain. Osteoarthritis often affects knees, hips, and hands, making mobility a daily struggle for many. Painkillers for osteoarthritis, such as NSAIDs and acetaminophen, are commonly prescribed to alleviate symptoms.
2. Fibromyalgia
A chronic disorder marked by widespread musculoskeletal pain, fatigue, and tenderness in localized areas. It’s often accompanied by sleep disturbances and cognitive difficulties. Due to its complex nature, painkillers for fibromyalgia might include a combination of medications like antidepressants and anticonvulsants to manage symptoms effectively.
3. Diabetic Neuropathy
A common complication of diabetes resulting in nerve damage primarily affecting the legs and feet. Symptoms include numbness, tingling, and sharp pains. Management may involve anticonvulsants or antidepressants tailored to nerve pain relief.
Considerations in Pain Management
The variability in chronic pain conditions requires personalized treatment plans that may incorporate different types of painkillers. While common painkillers are often the first line of defence, reliance solely on strong medications like strong painkillers for back pain may not always be effective or sustainable due to potential side effects.
Understanding these conditions is essential for developing targeted strategies that adequately address individual patient needs while minimizing reliance on traditional pharmacological treatments alone.
The Opioid Crisis: A Call for Non-Addictive Pain Management Options
The opioid crisis has become a significant public health emergency, affecting countless individuals and communities worldwide. This crisis stems from the widespread use and misuse of narcotic pain relievers, leading to tragic consequences such as addiction, overdose, and death. Opioid medications, initially prescribed for their potent pain-relieving properties, have a high potential for misuse due to their addictive nature.
The Impact of the Opioid Crisis
Individual Consequences
Many individuals find themselves trapped in a cycle of addiction after being prescribed opioids for legitimate medical reasons. The progression from therapeutic use to dependency can be rapid and devastating.
Societal Costs
The ripple effects extend beyond personal suffering. Families are torn apart, communities bear the brunt of increased healthcare demands, and economies are strained by lost productivity and increased healthcare costs.
Risks Associated with Narcotic Pain Relievers
Narcotic pain meds like oxycodone, hydrocodone, and morphine have been key contributors to this crisis. While effective in managing severe pain, these drugs carry significant risks:
- Addiction Concerns: Even short-term use can lead to physical dependence. Patients may experience withdrawal symptoms when attempting to discontinue use.
- Tolerance Development: Over time, patients often require higher doses to achieve the same level of pain relief, increasing the risk of overdose.
- Overdose Potential: High doses or improper use can result in respiratory depression, a potentially fatal condition.
By understanding these risks and impacts, it's clear that non-addictive alternatives are crucial for effective pain management without the drawbacks associated with opioids. These insights underscore the necessity of exploring safer options to address chronic pain while minimizing harm.
Non-Opioid Medications for Pain Relief: Exploring Effective Alternatives
Anticonvulsants: Targeting Nerve Pain with Gabapentin and Pregabalin
Anticonvulsants such as gabapentin and pregabalin have become important non-opioid options for pain management, particularly for nerve pain. Originally developed to treat epilepsy, these medications are now widely used for their ability to relieve nerve pain by regulating abnormal electrical activity in the nervous system.
How They Work:
- Gabapentin and pregabalin primarily target the central nervous system. They bind to specific subunits of voltage-gated calcium channels in the brain and spinal cord.
- By inhibiting excessive neuronal firing, these drugs help reduce the transmission of pain signals, which is especially beneficial for conditions involving nerve damage or dysfunction.
Common Uses:
- Chronic Conditions: Individuals suffering from chronic conditions such as diabetic neuropathy and postherpetic neuralgia often find relief with these medications.
- Fibromyalgia: Pregabalin is specifically approved for fibromyalgia, a condition characterized by widespread musculoskeletal pain along with fatigue, sleep, memory, and mood issues.
Advantages over Opioids:
- These medications provide an effective alternative to opioid pain relief by offering significant symptom reduction without the high risk of addiction or dependence associated with narcotic pain relievers.
- Their use reflects a shift towards non-opioid medications that focus on targeted symptom relief while minimizing systemic side effects.
While gabapentin and pregabalin are powerful tools in managing certain types of chronic pain, it's important to be aware of potential side effects such as dizziness or drowsiness. Collaborating closely with healthcare professionals ensures that these treatments are customized to individual needs, maximizing benefits while minimizing risks.
Anticonvulsants are just one part of a larger approach that includes various non-opioid options aimed at achieving effective and long-lasting pain management. For instance, exploring natural alternatives like those offered in our Pain Relief Bundle could provide additional ways to find relief. This bundle includes products designed to naturally alleviate back, joint, and muscle pain.
Furthermore, it's essential to understand that not all pain is caused by nerve damage or dysfunction. Conditions like atopic eczema and dermatitis can also result in significant discomfort. Gaining a better understanding of these conditions could enhance overall pain relief and management strategies.
Antidepressants in Chronic Pain Management: Beyond Mood Regulation
Antidepressants serve a dual purpose in chronic pain management, extending their benefits beyond mood regulation. Among these, serotonin/norepinephrine reuptake inhibitors (SNRIs) like duloxetine have gained attention for their role in alleviating chronic pain conditions such as fibromyalgia and diabetic peripheral neuropathy.
How SNRIs Work
SNRIs work by increasing the levels of serotonin and norepinephrine, neurotransmitters that play a critical role in signalling pathways related to pain perception. This modulation can lead to reduced pain signals being sent to the brain.
FDA Approval and Uses
Duloxetine is FDA-approved for treating both fibromyalgia and diabetic peripheral neuropathy, offering non-opioid pain control options for individuals suffering from these debilitating conditions.
The use of antidepressants highlights the broader category of non-opioid medications for pain relief, emphasizing that effective management doesn't solely rely on traditional opioid pain relief. By targeting different pathways involved in pain transmission, medications like duloxetine provide a comprehensive approach to managing chronic conditions.
Incorporating such strategies into treatment plans can enhance quality of life without the risks associated with narcotics, showcasing the potential of these nerve painkillers as part of a holistic approach to chronic pain management.
Topical NSAIDs: Localized Relief Without Systemic Side Effects
Topical nonsteroidal anti-inflammatory drugs (NSAIDs) offer a targeted approach to pain management, effectively addressing localized pain without the systemic exposure common in oral formulations. These medications are particularly beneficial for individuals seeking atopic pain relief without opioids, offering an alternative to traditional opioid pain relief methods.
One of the most widely used topical NSAIDs is diclofenac, known for its ability to alleviate pain associated with inflammatory conditions. Diclofenac works by inhibiting cyclooxygenase (COX) enzymes, thereby reducing the production of prostaglandins responsible for inflammation and pain. This mechanism allows it to serve as a potent inflammatory painkiller, targeting specific areas without the widespread side effects often linked to oral NSAID consumption.
The use of topical NSAIDs is advantageous for several reasons:
- Localized Action: Direct application means that the drug acts precisely where needed, providing targeted relief.
- Reduced Systemic Side Effects: By minimizing systemic absorption, these treatments decrease the risk of gastrointestinal issues and cardiovascular concerns associated with oral NSAIDs.
- Convenience and Safety: Easy application makes them accessible, promoting consistent use and adherence to treatment regimens.
For those dealing with chronic pain conditions such as osteoarthritis or localized musculoskeletal pain, topical NSAIDs like diclofenac present a viable non-opioid pain control strategy. They complement other non-opioid medications such as anticonvulsants (gabapentin and pregabalin) and antidepressants (duloxetine), broadening the spectrum of non-addictive pain management options available.
Innovative Approaches in Acute Pain Management: Intravenous Acetaminophen and Ibuprofen as Adjunct Therapies
In the world of treating severe pain, intravenous acetaminophen and ibuprofen are two powerful non-opioid medications that stand out. These pain relievers offer promising alternatives to traditional opioid medications, especially when quick and effective treatment is needed. Since they are given through an IV, they work quickly, making them perfect for situations like post-surgery recovery or emergencies.
How Intravenous Acetaminophen Works
Intravenous Acetaminophen works by blocking the production of certain chemicals in the body called prostaglandins, which are responsible for causing pain and fever. Unlike nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, acetaminophen does not have any risks of stomach problems associated with it. This makes it a safe option for patients who may be at risk for gastrointestinal issues.
The Role of Intravenous Ibuprofen
Intravenous Ibuprofen, on the other hand, is an NSAID that has strong anti-inflammatory and pain-relieving effects. It works by targeting specific pathways involved in inflammation and pain perception. This makes it an effective choice for conditions where inflammation is a significant contributor to pain.
Benefits of Using Both Medications Together
When used together, these two medications can provide even better pain relief than when used individually. This approach is known as multimodal pain management, where different types of medications are combined to target multiple mechanisms of action.
By using intravenous acetaminophen and ibuprofen as adjunct therapies alongside other treatments such as opioids or regional anaesthesia, healthcare providers can achieve:
- Improved Pain Control: The combination of these medications can enhance overall pain relief, allowing patients to be more comfortable during their recovery.
- Reduced Opioid Dependence: By minimizing the need for higher doses of opioids, this strategy can help prevent opioid-related side effects and complications.
- Individualized Treatment Plans: Every patient is unique, and tailoring interventions based on their specific needs can lead to better outcomes.
These innovative approaches in acute pain management demonstrate how integrating different non-opioid strategies can effectively address severe pain. They emphasize the importance of customizing treatments according to each patient's requirements, ultimately contributing to safer and more comprehensive pain management practices.
Non-Invasive Non-Pharmacological Therapies (NINPT) for Comprehensive Pain Relief Strategies
Harnessing Physical Modalities: TENS Therapy and Physical Therapy Techniques
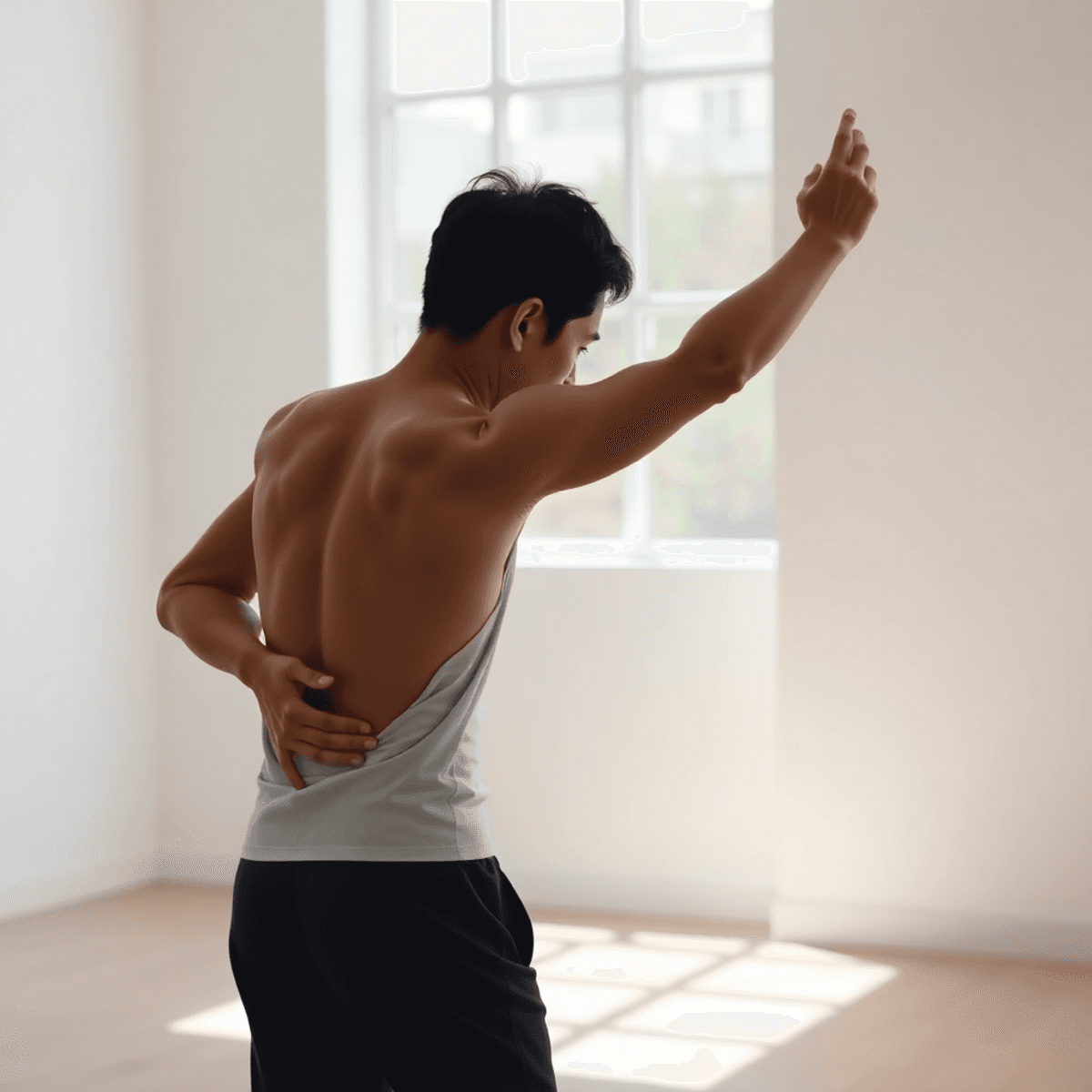
Transcutaneous Electrical Nerve Stimulation (TENS) therapy offers a promising non-narcotic pain relief option. It works by delivering low-voltage electrical currents through the skin to modulate pain signals. This method can effectively block the transmission of pain signals to the brain, providing atopic pain relief without opioids. The therapy has been shown to promote relaxation and reduce muscle tension, making it a suitable choice for individuals seeking non-addictive pain medicine.
While TENS therapy targets pain modulation, physical therapy techniques aim to improve overall function. These include:
- Strengthening exercises: Target specific muscle groups to enhance stability and support affected areas.
- Stretching routines: Increase flexibility, reducing stiffness and improving range of motion.
- Manual therapy: Involves hands-on techniques to manipulate soft tissues and joints, alleviating discomfort and enhancing mobility.
Physical therapists design personalized programs that address individual needs, focusing on restoring functional independence. Regular engagement in these activities can lead to significant improvements in mobility, enabling patients to manage chronic conditions more effectively.
Incorporating both TENS therapy and physical therapy into a comprehensive treatment plan allows for an integrative approach to pain management. This strategy not only addresses pain symptoms but also tackles underlying functional limitations, offering a holistic solution for those living with chronic pain conditions.
The Mind-Body Connection: Psychological Interventions in Chronic Pain Management
Addressing psychological factors is crucial in managing chronic pain. Emotional and mental stressors can intensify pain perception, complicating the healing process. Non-invasive non-pharmacological therapies (NINPT) offer a holistic approach, integrating both mind and body for effective pain relief.
Cognitive-Behavioral Therapy (CBT) plays a pivotal role in this strategy. As an evidence-based approach, CBT empowers individuals by helping them develop coping strategies and modify maladaptive thought patterns associated with their condition. By reshaping how one reacts to pain, CBT can lead to significant improvements in pain management outcomes.
Key Benefits of CBT
- Encourages positive thinking and resilience.
- Reduces reliance on non-narcotic painkillers.
- Complements other modalities like TENS therapy and physical therapy.
Incorporating CBT into a comprehensive treatment plan enables a more personalized approach to chronic pain management. It aligns well with atopic pain relief strategies by providing non-addictive pain medicine alternatives, addressing both the physical and psychological aspects of chronic conditions.
Exploring Complementary Therapies: Acupuncture and Yoga for Holistic Pain Relief
The world of non-invasive non-pharmacological therapies (NINPT) offers valuable options for managing chronic pain. Among these, acupuncture stands out by stimulating specific points on the body. This ancient technique aims to restore balance and promote healing, potentially offering relief without the risks associated with narcotic painkillers or non-addictive pain medicine.
How Acupuncture Works
Acupuncture works by targeting areas believed to influence pain pathways, thus enhancing the body's natural ability to heal itself. The practice may alter brain chemistry by affecting neurotransmitters and hormones involved in stress and pain responses, providing an effective method for atopic pain relief without opioids.
The Role of Yoga in Pain Management
On a different yet complementary path, yoga serves as a powerful tool in chronic pain management. By focusing on improving flexibility and reducing muscle tension, yoga fosters a heightened mind-body awareness. This holistic approach can significantly benefit individuals suffering from conditions like osteoarthritis or fibromyalgia.
- Improved Flexibility: Regular practice helps increase range of motion and joint health.
- Reduced Muscle Tension: Specific poses alleviate tension, aiding in relaxation.
- Mind-Body Awareness: Encourages mindfulness, helping manage pain perceptions more effectively.
A Comprehensive Strategy for Pain Relief
Both acupuncture and yoga contribute to a comprehensive strategy that avoids reliance on traditional narcotics or opioids while addressing chronic pain's multifaceted nature. In addition to these therapies, incorporating natural products can further enhance pain management. For instance, 1936 Original offers a range of products designed to help relieve back, joint, and muscle pain while reducing inflammation. These include their pain relief cream which is made from 95% natural ingredients sourced from the EU and has been family-made in Italy since 1936.
Emerging Non-Habit Forming Drugs: A Glimpse into Future Innovations in Pain Management
In the field of pain management, new types of drugs are emerging as promising alternatives to opioids. One such type targets specific receptors involved in pain control, namely the α2a-adrenergic receptor agonists. These medications are gaining attention for their potential to provide effective pain relief without the addictive qualities associated with traditional opioid treatments.
Understanding How α2a-Adrenergic Receptor Agonists Work
Recent research trends are delving into how these innovative treatments work. The α2a-adrenergic receptor agonists operate by engaging particular receptors in the nervous system that play a crucial role in modulating pain signals. By doing so, they can potentially alleviate pain without inducing sedation or other common side effects linked with opioid use. This mechanism offers an encouraging outlook for individuals seeking alternative solutions to manage chronic and atopic pain conditions.
Exploring the Therapeutic Potential and Safety of These Drugs
Current studies focus on understanding the therapeutic potential and safety profile of these drugs. Preclinical models have shown promising results, indicating that α2a-adrenergic receptor agonists might effectively reduce pain sensitivity and improve patient outcomes. As research progresses, there is hope that these compounds will offer a viable option for those struggling with chronic pain, paving the way for non-opioid-based therapies that prioritize safety and efficacy.
A Future Without Dependency
Innovation continues to drive the exploration of these non-habit-forming drugs, highlighting a future where effective pain management does not compromise patient well-being or lead to dependency. With ongoing advancements, the landscape of pain relief is poised for transformation, offering renewed hope for those affected by persistent pain conditions.
Integrating Multimodal Analgesic Approaches for Personalized Chronic Pain Management Plans
A multimodal approach to chronic pain management is essential in crafting a comprehensive strategy that leverages both pharmacological and non-pharmacological interventions. By utilizing a combination of treatments, healthcare professionals can optimize pain relief while diminishing the dependence on any single modality.
Combining Pharmacological and Non-Pharmacological Interventions
- Pharmacological Options: Non-opioid medications such as anticonvulsants, antidepressants, and topical NSAIDs each offer unique mechanisms of action. These can be strategically combined to target different aspects of pain pathways.
- Non-Invasive Non-Pharmacological Therapies (NINPT): Incorporating therapies such as Transcutaneous Electrical Nerve Stimulation (TENS), physical therapy, and psychological interventions enhances the overall treatment efficacy. These methods not only provide symptomatic relief but also address underlying factors contributing to chronic pain.
Tailoring Multimodal Analgesic Approaches
Personalization is key in multimodal strategies:
- Patient-Centric Plans: Treatment plans should reflect individual patient needs, preferences, and their specific response profiles. Considering factors like age, comorbidities, and lifestyle can guide clinicians in selecting the most appropriate combination of therapies.
- Dynamic Adjustments: Regular assessment of treatment effectiveness allows for modifications based on patient feedback and clinical observations. This adaptability ensures that the chosen modalities continue to meet evolving patient needs.
Integrating varied therapeutic options within a multimodal framework provides a robust foundation for effective chronic pain management. This strategy not only enhances pain control but also empowers patients through personalized care that aligns with their unique health journey.
Conclusion
Effectively managing chronic pain requires a shift towards non-opioid strategies that prioritize safety and effectiveness. By exploring various approaches such as anticonvulsants, antidepressants, topical NSAIDs, and innovative therapies, patients can achieve effective pain relief without relying on opioids. Non-invasive non-drug therapies further enhance these efforts, providing a holistic model for pain management. It is essential to emphasize personalized, multimodal treatment plans in order to reduce opioid dependency and address the specific needs of each individual. These comprehensive strategies will lead to sustainable and effective solutions for chronic pain relief.
FAQs (Frequently Asked Questions)
What are common types of chronic pain?
Common types of chronic pain include osteoarthritis, characterized by the breakdown of joint cartilage; fibromyalgia, marked by widespread musculoskeletal pain; and diabetic neuropathy, a complication of diabetes that results in nerve damage.
Why is there a need for non-opioid pain management options?
The opioid crisis has highlighted the significant public health emergency caused by addiction to narcotic pain relievers. Many individuals find themselves trapped in a cycle of addiction, leading to severe personal and societal costs. Non-opioid alternatives are essential for effective pain management without the risks associated with opioids.
What non-opioid medications are available for pain relief?
Effective non-opioid medications include anticonvulsants like gabapentin and pregabalin for nerve pain, antidepressants that also help manage chronic pain, topical NSAIDs for localized relief, and intravenous acetaminophen and ibuprofen as adjunct therapies for acute pain.
How can psychological interventions assist in managing chronic pain?
Psychological interventions such as Cognitive Behavioral Therapy (CBT) address emotional factors related to chronic pain. They encourage positive thinking, resilience, and reduce reliance on medication by helping patients develop coping strategies.
What role do complementary therapies play in holistic pain relief?
Complementary therapies like acupuncture and yoga contribute significantly to holistic pain relief strategies. Acupuncture targets specific areas believed to influence pain perception, while yoga promotes physical flexibility and mental well-being, enhancing overall pain management.
What is a multimodal approach to chronic pain management?
A multimodal approach integrates both pharmacological and non-pharmacological interventions tailored to individual needs. This strategy combines various treatment methods—such as medications, physical therapy, and psychological support—to create a comprehensive and personalized plan for managing chronic pain effectively.