21st Century Developments in Inflammatory Pain Treatment

Introduction
Inflammatory pain affects millions globally, significantly impairing daily activities and quality of life. Conditions like rheumatoid arthritis exemplify the debilitating nature of such pain, highlighting the need for effective treatment strategies. In the 21st century, developments in inflammatory pain treatment have aimed to alleviate these challenges.
Key areas of focus include:
- 21st-century developments in anti-inflammatory drugs: These advancements have introduced more targeted and safer options for managing inflammation.
- Personalised medicine approaches: Tailoring treatments to individual genetic and environmental profiles aims to optimise outcomes.
- Non-invasive diagnostic techniques: Enhancing early and accurate diagnosis through advanced imaging technologies.
- Future directions in research: Exploring novel therapeutic targets to revolutionise inflammatory pain management.
These innovations underscore a commitment to improving patient outcomes by addressing unmet needs in this critical area of healthcare.
1. Evolution of Anti-Inflammatory Drugs
The journey of anti-inflammatory drugs spans centuries, deeply rooted in both tradition and science. Initially, treatments for inflammatory conditions relied heavily on natural remedies. Salicylates, derived from willow bark, were among the earliest plant-based treatments known for their effectiveness in reducing joint inflammation and muscle pain. These natural compounds laid the groundwork for the development of aspirin, a synthetic derivative that became one of the most widely used over-the-counter anti-inflammatory medications.
The rise of non-steroidal anti-inflammatory drugs (NSAIDs) marked a significant leap in managing inflammatory conditions. NSAIDs offer a strong anti-inflammatory effect by inhibiting cyclooxygenase (COX) enzymes—key players in the inflammatory process. Understanding the distinct roles of COX-1 and COX-2 enzymes was pivotal. COX-1 is involved in maintaining normal physiological functions like protecting the stomach lining, while COX-2 is primarily responsible for inflammation and pain.
This insight led to the creation of selective COX-2 inhibitors, designed to minimise gastrointestinal side effects associated with traditional NSAIDs. Rofecoxib was one such innovation, acclaimed initially as one of the best anti-inflammatory options due to its targeted action. However, its later withdrawal from the market due to cardiovascular risks highlighted the delicate balance between efficacy and safety in drug development.
Key Milestones:
- Traditional Treatments: Salicylates from willow bark.
- Synthetic Advancements: Development of aspirin.
- NSAID Era: Introduction of drugs targeting COX enzymes.
- COX Enzyme Discovery: Differentiation between COX-1 and COX-2 roles.
- Selective Inhibitors: Launch and withdrawal of rofecoxib.
These developments underscore ongoing efforts to refine anti-inflammatory therapies, striving for effective solutions with reduced adverse effects. The evolution continues as researchers explore new pathways and mechanisms to alleviate inflammatory pain safely and efficiently.
2. Current Trends in Inflammatory Pain Treatment
Emerging trends in inflammatory pain management spotlight innovative approaches in drug discovery, particularly those targeting signal transduction pathways involved in inflammation. Signal transduction pathways play a crucial role in cellular communication and immune response, making them attractive targets for novel anti-inflammatory drugs.
1. New Anti-Inflammatory Drugs
These agents aim to modulate specific signalling molecules that propagate inflammatory signals, potentially offering more precise control over inflammatory processes. For instance, drugs inhibiting Janus kinase (JAK) pathways have shown promise in reducing inflammation with greater specificity.
2. Anti-Cytokine Therapies
Cytokines are proteins that mediate and regulate immunity and inflammation. Targeting cytokines has emerged as a promising strategy for managing chronic inflammatory diseases such as rheumatoid arthritis. Rheumatoid arthritis, specifically affecting the knee and other joints, benefits significantly from therapies like TNF-α blockers, which inhibit tumour necrosis factor-alpha, a key cytokine involved in the disease's pathogenesis.
Biologic therapies have revolutionised treatment protocols by targeting these specific mediators of inflammation. By selectively blocking cytokines or their receptors, these treatments reduce symptoms and slow disease progression more effectively than traditional therapies.
The focus on these advanced therapeutic strategies reflects a deeper understanding of underlying pathophysiological processes and the complexities of inflammatory diseases. By shifting towards targeted interventions, researchers aim to improve patient outcomes with fewer side effects, marking a significant advancement in the field of inflammatory pain treatment.
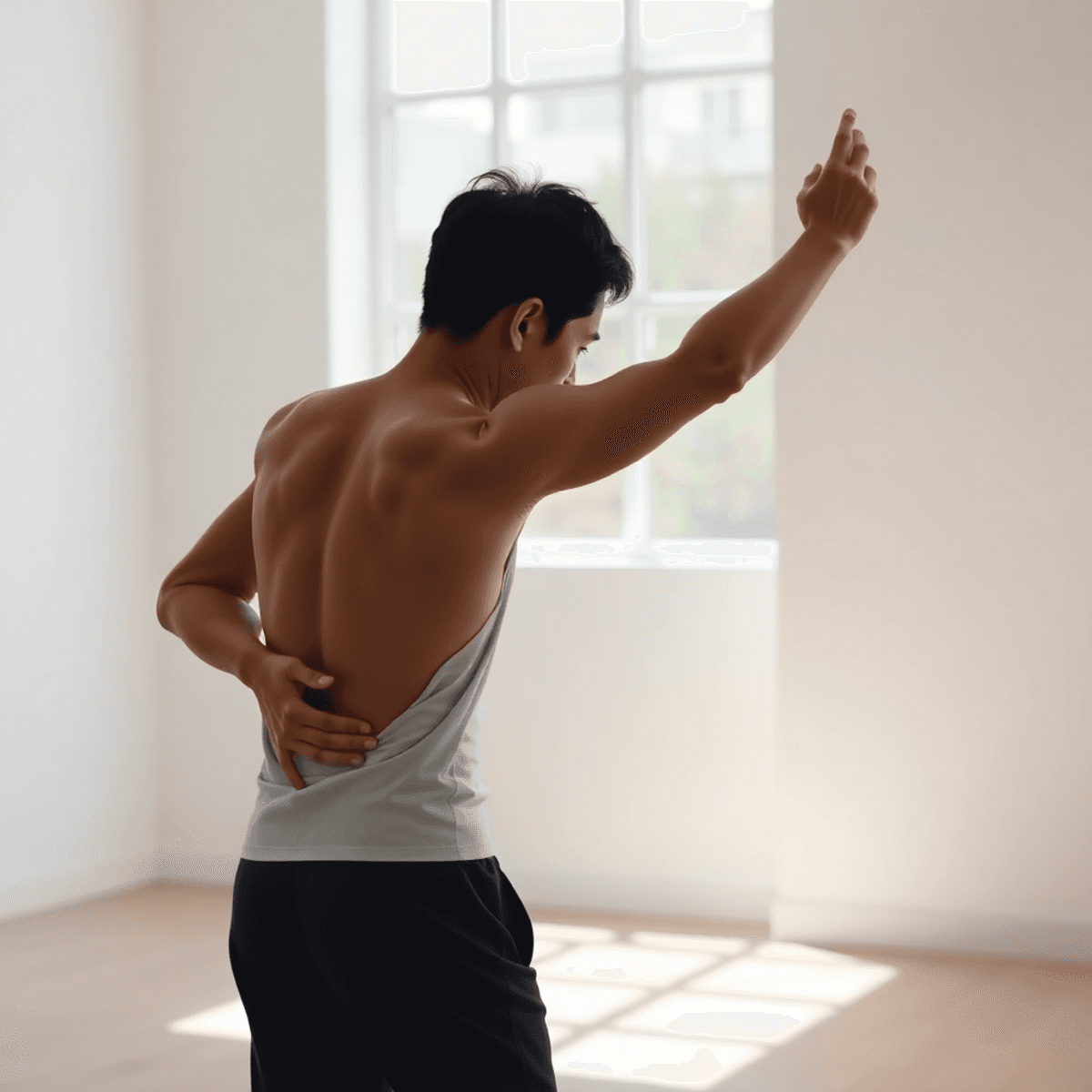
In addition to pharmaceutical innovations, there are also holistic approaches available that can help manage inflammatory pain. For instance, products designed to relieve back, joint and muscle pain using natural ingredients have been gaining popularity. These options offer an alternative or complementary approach to traditional medical treatments, focusing on reducing inflammation and providing relief from pain associated with conditions like rheumatoid arthritis.
3. Personalised Medicine in Inflammatory Pain Management
Personalised medicine is reshaping how inflammatory pain is managed, moving away from a one-size-fits-all approach to individualised treatment strategies. This shift is crucial because each patient's response to treatment can vary significantly based on numerous factors.
Tailoring Treatments
- Unique Characteristics: Each individual presents a distinct set of biological and environmental factors that influence the effectiveness of anti-inflammatory therapies.
- Genetic Predispositions: Advances in genomics have allowed researchers to identify specific genetic markers associated with how patients respond to certain medications.
Role of Genetic Markers
The identification of genetic markers has opened doors to tailor treatments more effectively. For instance, variations in genes responsible for drug metabolism can impact how well a patient responds to NSAIDs or biologics used in managing inflammatory conditions such as rheumatoid arthritis. By understanding these genetic differences, healthcare professionals can make informed decisions about which drugs might be most effective for each patient.
Environmental Influences
It's not just genetics that play a role; environmental factors also contribute to treatment efficacy. Lifestyle choices, diet, and exposure to environmental triggers can alter an individual's inflammatory pathways, necessitating adjustments in therapeutic approaches.
The 21st-century developments in the treatment of inflammatory pain underscore the importance of these personalised approaches. By integrating insights from genetic predispositions and environmental contexts into clinical practice, healthcare providers can enhance patient outcomes and reduce adverse effects associated with inappropriate therapy choices. This paradigm shift towards personalisation represents a significant advancement in optimising care for individuals suffering from inflammatory pain.
4. Non-Invasive Diagnostic Techniques for Inflammatory Diseases
Recent advancements in non-invasive imaging technologies are transforming the diagnostic landscape for inflammatory diseases. These innovations enhance accuracy and enable early detection, crucial for effective treatment planning. Key imaging techniques include:
- Magnetic Resonance Imaging (MRI): Provides comprehensive views of soft tissues, helping identify inflammation in joints and organs without radiation exposure.
- Ultrasound: Offers real-time visualisation of tissues and can detect subtle changes associated with inflammation, beneficial for conditions like rheumatoid arthritis.
- Positron Emission Tomography (PET): When combined with CT or MRI, PET scans reveal metabolic activity linked to inflammatory processes, providing functional insights.
Leveraging these advanced diagnostic capabilities allows clinicians to tailor interventions more precisely and monitor the effectiveness of treatments over time. This evolution in diagnostic approaches underscores the potential for improved patient outcomes through early and accurate identification of inflammatory conditions.
5. Future Directions in Inflammatory Pain Research
The future of inflammatory pain research is set to expand beyond the traditional framework of anti-inflammatory drugs, with ongoing research exploring new therapeutic targets. Innovations in this field are poised to revolutionise how inflammatory pain, including inflammatory back pain, is managed.
Key areas of interest include:
- Molecular Pathways: Investigating molecular pathways involved in inflammation opens doors for novel drug targets. By understanding these pathways, researchers aim to develop therapies that precisely modulate the body's inflammatory response without adverse side effects.
- Biologics and Beyond: The success of biologics such as TNF-α inhibitors has paved the way for next-generation treatments. Scientists are now looking into other cytokines and cellular interactions as potential therapeutic targets.
- Gene Therapy and Regenerative Medicine: These emerging fields offer promising avenues for long-term relief from chronic inflammation. Efforts are directed towards restoring normal tissue function by correcting underlying genetic defects or promoting tissue regeneration.
The integration of these innovative approaches highlights the potential to transform patient outcomes significantly, offering hope for more effective and tailored treatments in the future. For instance, alongside these advancements, products like aspirin-free pain relief cream are already providing targeted relief for those suffering from various forms of pain, including back and joint pain, while reducing inflammation effectively.
Conclusion
Ongoing research and development are essential in meeting the unmet needs of inflammatory pain treatment. Advancements in pain management in the 21st century have paved the way for new and innovative therapies, but there is still much work to be done. By staying informed about these emerging therapies, you can take an active role in your healthcare journey.
The field of inflammatory pain management is constantly evolving, with new therapeutic targets being explored. This means that there are always new options and possibilities for improving your condition. By staying engaged and educated about these developments, you can make informed decisions that enhance your quality of life.
In summary, it is crucial to stay updated on the latest advancements in inflammatory pain treatment. This knowledge will empower you to advocate for yourself and seek out the best possible care. Remember, you have the power to shape your own healthcare journey.
FAQs (Frequently Asked Questions)
What is inflammatory pain and how does it affect individuals globally?
Inflammatory pain is a type of pain that arises from inflammation, affecting millions of people worldwide. It can significantly impact quality of life, leading to chronic discomfort and disability in various populations.
How have anti-inflammatory drugs evolved over the years?
The evolution of anti-inflammatory drugs spans centuries, beginning with traditional remedies and progressing to modern pharmaceuticals that target specific pathways involved in inflammation. This journey reflects advancements in our understanding of inflammatory processes and drug development.
What are some current trends in the treatment of inflammatory pain?
Current trends in inflammatory pain treatment include the introduction of new anti-inflammatory drugs that modulate specific signalling molecules, the development of anti-cytokine therapies which target proteins regulating immunity, and the application of personalised medicine approaches to tailor treatments based on individual patient characteristics.
Why is personalised medicine important in managing inflammatory pain?
Personalised medicine is crucial because it allows for tailored treatments that consider unique patient characteristics, including genetic markers and environmental influences. This approach enhances treatment efficacy and minimises adverse effects by aligning therapies with individual biological profiles.
What advancements have been made in non-invasive diagnostic techniques for inflammatory diseases?
Recent advancements in non-invasive imaging technologies have significantly improved the diagnosis of inflammatory diseases. These techniques enable healthcare providers to assess inflammation without the need for invasive procedures, leading to better patient outcomes and monitoring.
What does the future hold for research in inflammatory pain treatment?
The future of inflammatory pain research is poised for expansion, focusing on innovative therapies, improved diagnostic methods, and a deeper understanding of underlying mechanisms. Ongoing research and development are essential to meet the evolving needs of patients suffering from inflammatory pain.